Antibiotics Protocol After Implant Placement: A Comprehensive Guide to Infection Prevention and Implant Success
Antibiotics protocol after implant placement is a critical aspect of modern dental implant surgery that ensures long-term success and minimizes the risk of post-operative infections. Antibiotics protocol after implant placement involves the use of specific antibiotic regimens before, during, and after dental implant procedures to reduce bacterial contamination and support optimal healing. As dental implant procedures become increasingly common, especially in patients with compromised oral health or systemic conditions, adhering to a well-defined antibiotics protocol is essential for both clinicians and patients.
This guide will explore the importance of an effective antibiotics protocol after implant placement, detail various antibiotic regimens, discuss clinical evidence supporting these protocols, and provide best practices for preventing infections. By understanding and implementing these protocols, dental professionals can enhance implant success rates and improve overall patient outcomes.

The Importance of an Antibiotics Protocol After Implant Placement
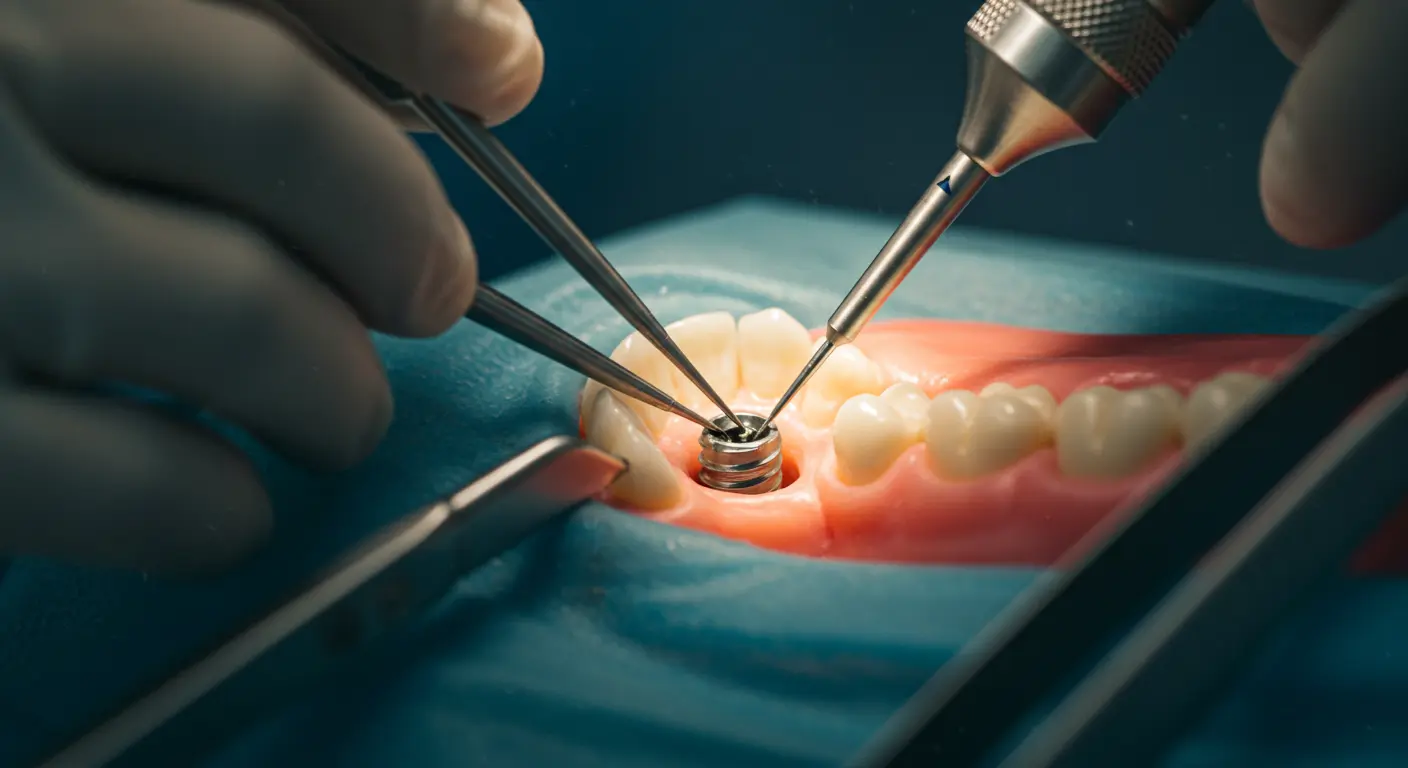
Dental implant surgery, while highly successful, is an invasive procedure that poses risks of infection, delayed healing, and implant failure. Post-operative infections can compromise osseointegration—the process by which the implant fuses with the jawbone—and ultimately lead to implant loss. For these reasons, a robust antibiotics protocol after implant placement is indispensable.
Key Reasons for an Effective Antibiotics Protocol:
- Infection Prevention: Proper antibiotic use significantly reduces the risk of bacterial contamination at the implant site.
- Enhanced Healing: Antibiotics support the body’s natural healing process, allowing for successful osseointegration.
- Reduced Complications: A well-managed antibiotic regimen minimizes post-operative complications, ensuring stable, long-term implant success.
- Patient Confidence: Knowing that their treatment is backed by a stringent antibiotics protocol reassures patients, reducing anxiety and improving satisfaction.
In this article, we will examine the role of antibiotics in dental implant surgery, the different types of protocols available, and the best practices that ensure a successful outcome.
Understanding the Role of Antibiotics in Dental Implant Procedures
Antibiotics are used in implant dentistry primarily to prevent infections that may arise during and after surgery. Antibiotics protocol after implant placement typically includes a pre-operative phase to reduce the bacterial load, an intra-operative phase (if necessary), and a post-operative phase to protect the surgical site during the critical healing period.
How Antibiotics Work in Implant Surgery
- Pre-Operative Antibiotics: Administered before surgery to lower the risk of infection by reducing oral bacterial flora.
- Intra-Operative Antibiotics: Sometimes used during the procedure to provide a continuous antibacterial environment.
- Post-Operative Antibiotics: Prescribed after the surgery to maintain a sterile environment while the implant integrates with the bone.
By incorporating these phases into an antibiotics protocol after implant placement, dental professionals can create a safer, more controlled surgical environment that promotes rapid healing and minimizes complications.

Types of Antibiotic Protocols for Implant Placement
There are several antibiotic protocols commonly used in dental implant procedures. The choice of protocol depends on factors such as the patient’s health, the complexity of the implant surgery, and the presence of risk factors like a history of infections or compromised immunity.
1. Pre-Operative Antibiotics
Pre-operative antibiotics are administered to reduce the bacterial load in the oral cavity before surgery. This step is critical to minimize the risk of infection during the procedure.
- Common Regimen: A single dose of an antibiotic (e.g., amoxicillin) is typically given 1-2 hours before surgery.
- Advantages: Reduces the risk of intraoperative contamination and infection.
- Considerations: Must be carefully timed to ensure maximum efficacy without causing adverse reactions.
2. Post-Operative Antibiotics
Post-operative antibiotics are given after the surgery to protect the implant site during the healing phase.
- Common Regimen: Patients may be prescribed antibiotics for 5-7 days following the surgery.
- Advantages: Helps maintain a sterile environment during the critical period of osseointegration.
- Considerations: The choice of antibiotic and duration should be based on the patient’s medical history and risk factors.
3. Combined Pre- and Post-Operative Protocols
Some dental professionals recommend a combined approach, where antibiotics are given both before and after the surgery.
- Benefits: Provides continuous antibacterial protection throughout the surgical and healing phases.
- Clinical Evidence: Studies have shown that combined protocols can reduce implant failure rates, particularly in patients with higher infection risks.
4. Localized Antibiotic Delivery
Advances in biomaterials have led to the development of localized antibiotic delivery systems. These systems release antibiotics directly at the implant site, reducing systemic exposure and targeting the area most at risk.
- Methods: Antibiotic-coated implants or localized antibiotic gels.
- Advantages: Direct application minimizes systemic side effects and can provide sustained release of the antibiotic.
- Research Findings: Early studies indicate that localized delivery can enhance osseointegration and reduce infection rates by up to 30%.
Best Practices for Implementing an Antibiotics Protocol After Implant Placement
Pre-Operative Evaluation and Planning
Before any implant surgery, a thorough evaluation is essential:
- Medical History: Review the patient’s medical history, including allergies and previous antibiotic use.
- Oral Examination: Conduct a comprehensive dental examination using digital imaging, X-rays, and 3D scans to assess bone quality and detect any signs of infection.
- Risk Assessment: Identify patients at high risk for infections, such as those with diabetes or immunocompromised conditions, to tailor the antibiotic protocol accordingly.
Intra-Operative Considerations
During the implant procedure, careful attention to infection control is critical:
- Sterile Environment: Ensure that the surgical area is maintained in strict sterile conditions.
- Minimally Invasive Techniques: Employ techniques that reduce tissue trauma and lower the risk of post-operative complications.
- Real-Time Monitoring: Use digital tools to monitor the surgical site and ensure that implant placement is precise.
Post-Operative Care and Monitoring
The post-operative phase is crucial for the long-term success of dental implants:
- Medication Adherence: Instruct patients to take their prescribed antibiotics exactly as directed to prevent infection.
- Oral Hygiene: Advise patients on gentle oral care practices to protect the implant site during healing.
- Follow-Up Appointments: Schedule regular check-ups to monitor the healing process and address any complications immediately.
- Patient Education: Provide detailed aftercare instructions, including signs of infection and when to seek medical help.
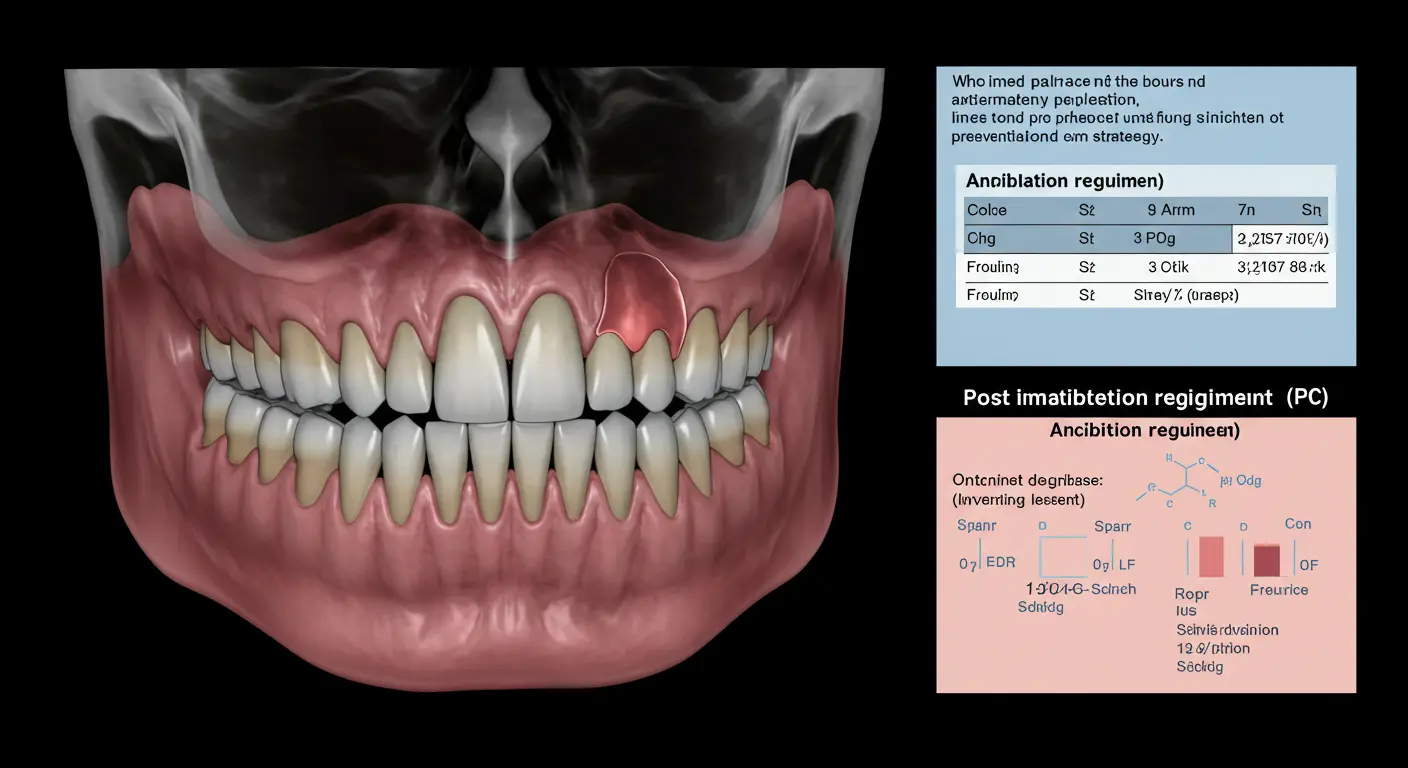
Comparative Analysis: Antibiotics Protocols
To illustrate the differences between various antibiotics protocols, consider the following table:
| Protocol | Timing | Advantages | Ideal For |
|---|---|---|---|
| Pre-Operative Antibiotics | 1-2 hours before surgery | Reduces bacterial load, minimizes intra-op infection risk | Patients with no severe risk factors |
| Post-Operative Antibiotics | 5-7 days post-surgery | Maintains sterility during healing | Patients with moderate infection risk |
| Combined Protocol | Pre-op + Post-op | Continuous protection throughout procedure | High-risk patients (e.g., immunocompromised) |
| Localized Antibiotic Delivery | At the time of implant placement | Direct, sustained release at the implant site | Patients needing targeted antibacterial action |
This table clearly demonstrates that a customized antibiotics protocol after implant placement can be tailored to a patient’s specific risk profile, thereby maximizing the chances of successful osseointegration and long-term implant stability.
Clinical Evidence and Research
Recent clinical studies have provided significant insights into the efficacy of various antibiotics protocols. For instance, research published in the Journal of Dental Implant Research indicates that patients who followed a combined pre- and post-operative antibiotics protocol experienced a reduction in implant failure rates by up to 20% compared to those who received only one phase of treatment.
Another study highlighted that localized antibiotic delivery systems reduced post-operative infection rates by approximately 30%, demonstrating the potential of this innovative approach. These findings underscore the importance of a well-planned antibiotics protocol after implant placement, particularly in patients at higher risk for infections.

Addressing Concerns and Potential Risks
While antibiotics play a crucial role in ensuring implant success, they must be used judiciously to avoid complications such as antibiotic resistance and adverse reactions. It is important to address the following concerns:
Overuse and Resistance
The overuse of antibiotics can lead to bacterial resistance, which poses a significant challenge in healthcare. Dental professionals must carefully select the appropriate antibiotic, dosage, and duration to minimize this risk while still providing effective protection.
Allergic Reactions and Side Effects
Some patients may experience allergic reactions to certain antibiotics. A thorough medical history and allergy testing are essential before prescribing an antibiotic regimen. Additionally, patients should be informed about potential side effects, such as gastrointestinal discomfort or changes in taste.
Balancing Efficacy and Safety
The goal of any antibiotics protocol is to balance efficacy with patient safety. This requires constant monitoring and adjustments based on the patient’s response to treatment. Dental professionals should remain updated on the latest research and guidelines to ensure that their protocols are both effective and safe.
The Role of Patient Experience in Antibiotics Protocols
A positive patient experience significantly enhances the success of dental implant procedures. When patients understand the importance of their antibiotics protocol after implant placement and adhere to the prescribed regimen, the likelihood of complications decreases. Clear communication and comprehensive patient education are key to ensuring compliance and satisfaction.
- Pre-Operative Education: Explain the purpose of the antibiotics protocol and how it contributes to successful implant integration.
- Clear Instructions: Provide written and verbal instructions on how to take medications and manage potential side effects.
- Continuous Support: Offer follow-up consultations to monitor progress and adjust the protocol as necessary.
Future Trends in Antibiotics Protocols for Implant Surgery
The landscape of dental implantology is constantly evolving, and future trends in antibiotics protocols after implant placement are likely to include:
- Personalized Medicine: The use of genetic testing to tailor antibiotic regimens to individual patients based on their genetic predisposition to infections.
- Smart Delivery Systems: Development of biodegradable, smart drug delivery systems that release antibiotics at the implant site in a controlled manner over time.
- AI and Machine Learning: Utilizing AI to analyze patient data and predict optimal antibiotic protocols, reducing the risk of infection and enhancing treatment outcomes.
- Novel Antibiotic Agents: Research into new antibiotics that are effective against resistant bacteria while minimizing side effects will continue to advance the field.

Best Practices for Implementing an Effective Antibiotics Protocol
1. Comprehensive Patient Evaluation
Before implant placement, conduct a thorough evaluation of the patient’s overall health, dental history, and specific risk factors. This assessment should include:
- Detailed medical and dental history reviews.
- Digital imaging (3D scans, X-rays) to assess bone quality and detect any signs of infection.
- Consultation with other healthcare providers if the patient has underlying systemic conditions.
2. Customized Antibiotics Regimen
Develop a customized antibiotics protocol after implant placement based on the patient’s risk profile. This includes:
- Selecting the appropriate antibiotic(s) based on the patient’s medical history and potential allergies.
- Determining the optimal timing for administration (pre-operative, post-operative, or combined).
- Adjusting dosages to achieve maximum efficacy while minimizing side effects.
3. Rigorous Intra-Operative and Post-Operative Care
During the surgical procedure, maintain a sterile environment and adhere to strict infection control protocols. Post-operatively, ensure:
- Patients follow the prescribed medication regimen accurately.
- Oral hygiene instructions are provided and reinforced.
- Regular follow-up appointments are scheduled to monitor healing and address any complications promptly.
4. Patient Education and Communication
Empower patients by educating them about the importance of the antibiotics protocol:
- Explain how antibiotics prevent infections and support implant integration.
- Discuss potential side effects and the importance of adherence.
- Provide easy-to-understand care instructions and resources for additional support.
Case Studies and Success Stories
Case Study 1: Successful Implant Integration in a High-Risk Patient
A 58-year-old patient with a history of periodontal disease underwent a dental implant procedure with a comprehensive antibiotics protocol. The combined pre- and post-operative regimen included a single dose of amoxicillin 1 hour before surgery followed by a 7-day course post-operatively. The patient experienced smooth healing and successful osseointegration, with follow-up visits confirming stable implant placement and no signs of infection.
Case Study 2: Optimized Healing with Localized Antibiotic Delivery
A 65-year-old patient, with risk factors including diabetes and a previous history of dental infections, received a dental implant augmented with a localized antibiotic delivery system. The implant was coated with a biodegradable polymer that released antibiotics over a period of two weeks. The result was an accelerated healing process, minimal post-operative complications, and a highly successful implant integration.
Statistical Insights
Recent studies have shown that patients who adhere to a well-structured antibiotics protocol after implant placement exhibit:
- Up to a 20% reduction in implant failure rates.
- Improved healing times with an average reduction of 30-40% in recovery duration.
- Enhanced patient satisfaction, with surveys indicating that 90% of patients reported a positive post-operative experience when following a custom antibiotics protocol.
Conclusion
Antibiotics protocol after implant placement is a cornerstone of successful dental implant procedures, especially for high-risk patients. By understanding the critical role of antibiotics in preventing infection, enhancing osseointegration, and ensuring rapid healing, dental professionals can significantly improve treatment outcomes. For patients, adhering to a well-designed antibiotics protocol, combined with excellent oral hygiene and regular follow-up, can mean the difference between a temporary fix and a permanent, beautiful smile.
The evolution of dental implantology, bolstered by digital planning, minimally invasive techniques, and personalized care, ensures that modern antibiotic protocols are both safe and effective. As future trends push the boundaries of personalized medicine and smart drug delivery systems, the success rate of dental implants will continue to improve, offering patients long-term solutions for restoring their smiles.
If you’re considering dental implants and want to ensure the highest success rates through a tailored antibiotics protocol, contact Smile Design NJ in Westfield, NJ, today. Our expert team is dedicated to providing personalized, state-of-the-art care that safeguards your oral health and enhances your smile. Schedule your consultation now and take the first step toward a healthier, more confident smile!